As summer fades and temperatures begin to cool down, you may be looking forward to enjoying the fall foliage and spending time in the great outdoors. This could mean more opportunity to brush with black-legged ticks, the irksome creatures known for the spread of Lyme disease.
If you live in a highly endemic area such as Virginia, or elsewhere along the East Coast, you know you need to grab more than a pumpkin spice latte before heading off on a morning hike through the wooded trails.
Proper clothing and chemical repellent can help prevent tick bites and tick-borne illness. But did you know that Lyme disease can cause complications far greater than flu-like symptoms or a bullseye rash? Lyme disease can have a profound effect on mental health, especially if left untreated.
Dr. Robin Ridinger is a double-board-certified physician, whose expertise in Lyme Disease treatment is unparalleled. Based in Leesburg, Virginia, Dr. Ridinger utilizes a highly personalized, healing-oriented approach to her functional medicine practice. She takes the whole person into account, including all aspects of their lifestyle and full medical history.
Have concerns about Lyme disease? Contact Dr. Ridinger for a Lyme disease consultation.
Understanding the Basics of Lyme Disease
Lyme disease is a highly frustrating disease and unfortunately one of the least understood conditions in modern medicine. Ticks carry a wide array of microbes that can wreak havoc on any number of organs and systems in the human body.
When a tick bites, microbes such as Borrelia burgdorferi (also known as B. burgdorferi – the microbe associated with Lyme disease) are transmitted to the host. Often the individual doesn’t know they have been bitten, because the tick may even drop off before it is ever detected.
One of the first symptoms, and probably the most widely recognized, is the bullseye rash—the circular, expanding rash that looks like a target. This, accompanied by flu-like symptoms are considered hallmark indicators of the presence of Lyme. If detected early on, most individuals respond well to treatment with antibiotics and live happily ever after.
Oh, how we wish that was the end of the story! Unfortunately, it is not always the case.
If you have concerns about a tick bite or bullseye rash, schedule a consultation today.
Mighty Microbes are a Stealthy Matter
Microbes such as B. burgdorferi are stealthy and able to adapt. Their corkscrew shaped bacterium (spirochetes) can burrow deep within muscles and organs, even taking up residence in the brain and spinal cord. They can be hard to find and even harder to get rid of. Individuals with a robust immune system may successfully stave off infection, never knowing that microbes are lurking deep within their tissue waiting for an opportunity to rise in number causing chaos and disease.
For others, the presence of such microbes can cause chronic illness. Though it may not be life-threatening, feeling like you have the flu every day for weeks or months on end is demoralizing and overall can make for a miserable existence.
Symptoms may include:
- Chronic fatigue
- Body aches (myalgia)
- Joint pain (arthralgia)
- Nerve pain (neuralgia)
- Fever and chills
- Swollen lymph nodes
- Poor sleep
- Brain fog
- Headaches
- Dizziness
- Heart palpitations
- Depression, mood swings and personality changes
- Encephalopathy (generalized brain dysfunction)
Lyme Disease’s Neurological Effects
Depression is a common symptom of many chronic illnesses and Lyme disease is no exception. It’s no wonder that depression is associated with chronic illness, especially when it comes with a long list of symptoms. It is not uncommon for patients to endure months or even years battling chronic illness without identifying the root cause. Walking this arduous road can be exhausting and demoralizing, especially when healthcare providers are baffled and unable to provide much-needed answers.
Unfortunately, it’s not uncommon for patients to be told that their symptoms are psychosomatic or to be given antidepressants without the benefit of addressing the underlying cause.
Lyme Literate Medical Doctors (LLMD) such as Dr. Robin Ridinger understand that tick-borne illnesses can affect mental health in ways that extend beyond one’s ability to cope or persevere under the pressure of declining quality of life.
Depression and anxiety are certainly understandable; however, there may be physiological reasons behind those feelings. In fact, it is possible for microbes such as B. burgdorferi to cross the blood-brain barrier and affect the central, peripheral and autonomic nervous systems.
That is why it is imperative to find a highly trained medical doctor who listens without judgment and is not quick to attribute symptoms to psycho-social or behavioral issues or just plain stinking thinking.
Crossing the Blood-Brain Barrier
You may be wondering, “What is this blood-brain barrier and why is it important?” In the most simplistic terms, the blood-brain barrier is like a rubber swim cap that protects the brain and its functions from foreign invaders. When this barrier has been compromised, it is like trying to swim with a dew rag to protect your hair. There’s a good chance you will get wet and things may get messy.
Fortunately, LLMDs such as Dr. Ridinger understand which antibiotics and anti-inflammatory medications are capable of also crossing the blood-brain barrier and hunting down these crafty intruders. While much research still needs to be done, it stands to reason that any infection that can cause inflammation of the brain (encephalitis), has the potential to produce psychiatric disorders as well as other neurological symptoms.
Before you panic at the thought of microbes attacking your brain like alien invaders in a science fiction movie, it is important to note that the presence of neurological symptoms does not necessarily mean the blood-brain barrier has been compromised by infection.
Brain imaging of patients with encephalopathy (generalized brain dysfunction) can reveal areas of decreased blood flow and physiological changes which may be causing symptoms. Your skilled LLMD can help understand the root of what is going on and chart a course to restore quality of life.
Signs and Symptoms of Neuroinflammation
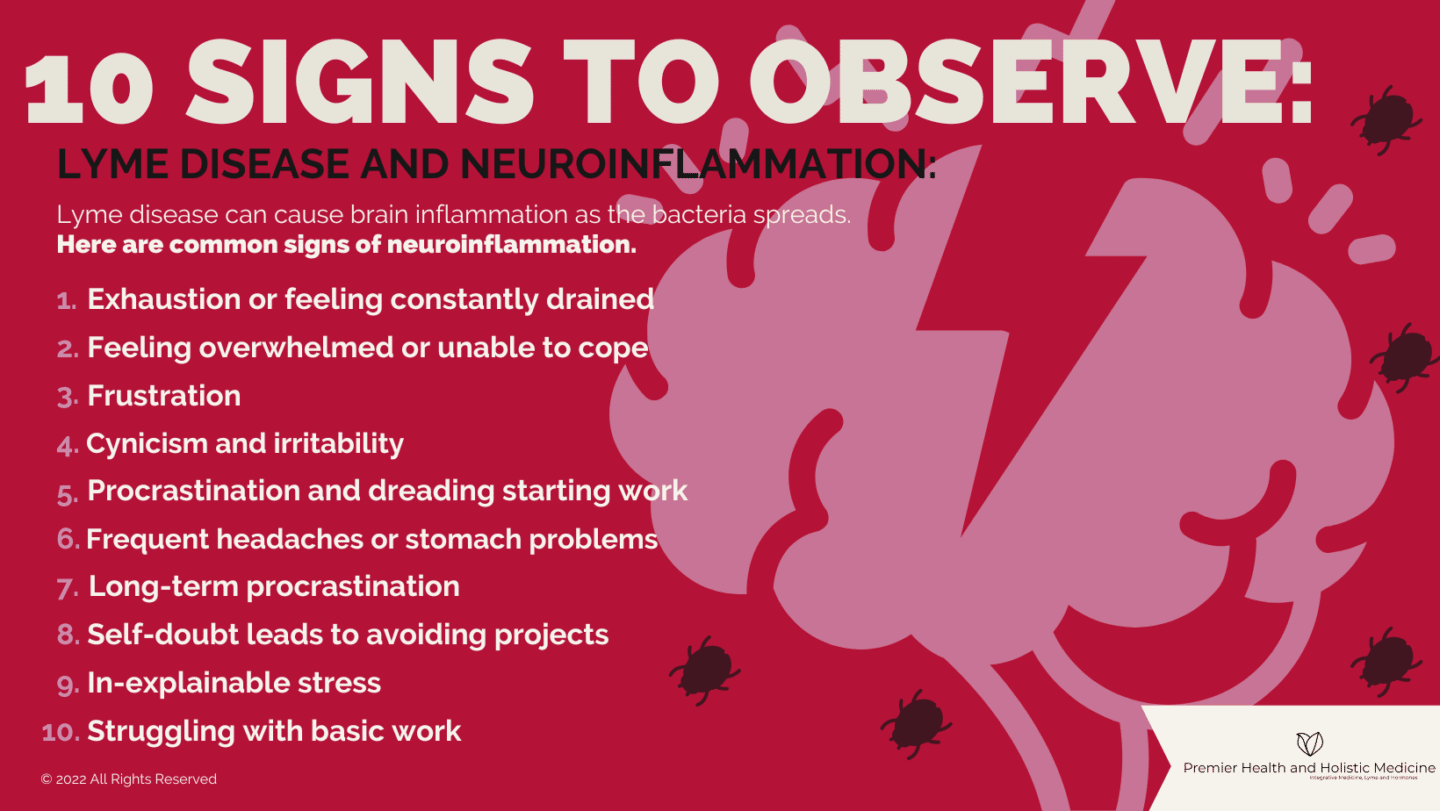
The onset of neurological symptoms can occur as early as one week to two months following a tick bite. Yet it is possible for symptoms to begin manifesting before Lyme disease is detectable by a blood test. Inflammation of the brain can cause a wide array of symptoms such as:
- Headaches
- Nausea/ vomiting
- Vertigo
- Meningitis
- Neck stiffness
- Facial palsy (Bell’s palsy)
- Depression or anxiety
- Personality changes and mood swings
- Irritability
- Visually tracking words on a page
- Memory impairment
- Speech difficulties
- Confusion, brain fog or “Lyme brain”
- Hallucinations (auditory or visual)
Such symptoms can be frightening and oftentimes are misdiagnosed or attributed to the wrong cause. Because of the stealthy nature of tick-borne microbes, symptoms may appear, reappear and evolve over the course of months or even years. Unfortunately, there is no standard progression charting the course of what Lyme disease should look like. Every case is unique. The one thing they do have in common is chaos.
Speak to your doctor if you are experiencing physiological, cognitive or neurological symptoms affecting your quality of life.
Hope for the Fight Against Chronic Illness
It stands to reason that because Lyme is a bacterial infection, you cannot improve cognitive function without first killing the bacteria that is responsible for the infection. This may sound over-simplistic, especially considering the complexity of the human body.
However, Dr. Robin Ridinger has a wide array of treatments and modalities in her arsenal to help fight Lyme disease and its associated symptoms – for example, she may incorporate antibiotics to combat the bacterium, while monitoring the effects that die-off can produce. Dr. Ridinger may simultaneously use other modalities to help bring the patient’s body back into a state of homeostasis where systems are able to function at peak performance.
The more robust a person’s immune system is, the greater he or she can fight the battle against chronic illness and secondary infections. That is why Dr. Ridinger uses a holistic approach to treatment. Her broad scope of personalized functional medicine includes optimizing health, wellness, sleep, and nutrition, decreasing chemical and toxin exposure, and supporting whole-body detoxification.
Dr. Robin Ridinger is Your Premier Choice for Healthcare
Treatment for Lyme disease is more effective if begun early. Dr. Ridinger has more than 10 years of experience in diagnosing and treating Lyme disease. She understands the challenges and frustrations her patients feel. She is committed to compassionately guiding her patients on a personalized journey to restored health and wholeness.
If you think you have signs and symptoms of Lyme disease — particularly if you live in an area where Lyme disease is common — contact a Lyme disease specialist. Request an appointment at Premier Health and Holistic Medicine today.