Spring has sprung and the glorious sunshine seems to beckon us all to spend more time outdoors. Whether you enjoy hiking, spending a sunny day at the park or conquering spring cleanup chores in your own backyard, it’s important to be mindful of those tiny pests: ticks.
While not all ticks carry Lyme disease, if you’ve been bitten by a tick or are experiencing flu-like symptoms after a tick bite, it may be advisable to see your family medical practitioner as soon as possible. Dr. Robin Ridinger is a double-board-certified physician, based in Leesburg, Virginia and expert in Lyme disease treatment. Her healing-oriented, personalized functional medicine practice takes into account the whole person including all aspects of their lifestyle.
Have concerns about a tick bite? Contact Dr. Ridinger for a Lyme disease consultation.
I Have a Tick Bite. Should I Be Concerned?
The chances of contracting Lyme disease from a single tick bite are slim, and according to the CDC, it depends on factors such as the type of tick, where you acquired it, and how long it was attached. Not all ticks carry the Borrelia burgdorferi bacteria, and a mere brush with a tick will not spread Lyme disease. Ticks must attach themselves to a host and indulge in a blood meal in order to spread the bacteria that causes Lyme disease.
Fortunately, your risk is very low if a tick has been attached for fewer than 24 hours, so it is imperative to check your body daily to both see and feel if ticks are present. If a tick has indeed attached itself, remove it with fine-tooth tweezers as soon as possible.
Has a tick bitten you? Schedule a visit for a consultation.
Can I Get Lyme Disease Anywhere in the U.S.?
Ticks can be found across the United States and do carry a variety of bacteria responsible for other diseases. However, Lyme disease is the only tick-borne illness associated with joint pain, arthritis, neurological issues and paralysis.
Blacklegged ticks are the only species to transmit the Borrelia burgdorferi bacteria responsible for Lyme disease and only those found in highly endemic areas of the northeastern and north central U.S. are commonly infected. Most infections reported in the U.S. occur or can be traced back to travel in the following endemic areas:
- Northeast and Mid-Atlantic, from Virginia to Maine
- North Central states, mostly in Wisconsin and Minnesota
- West Coast, particularly northern California
How Can I Prevent Lyme Disease?
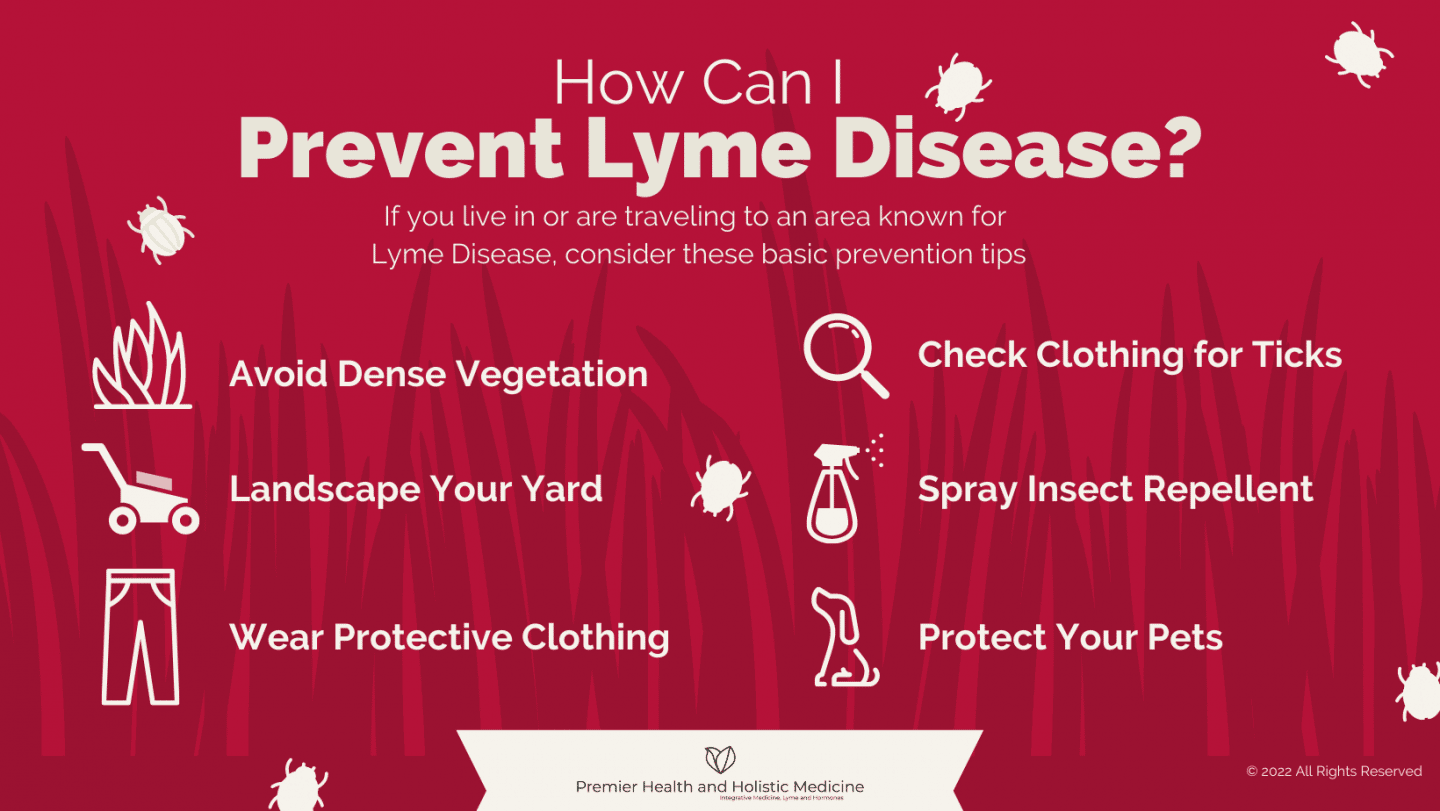
Lyme disease cases are sometimes diagnosed and reported from unexpected places, but they are almost always travel-related. If you live in or are traveling to an endemic area, consider these basic Lyme Disease prevention tips:
- Avoid Dense Vegetation: Ticks prefer tall, grassy or bushy areas, where they can easily hop onto passersby. If you are hiking or playing outdoors, avoid those areas and instead keep along the cleared path where ticks are less likely to be.
- Landscape Your Yard: Regularly mowing and landscaping your yard is an excellent measure for keeping you, your family and pets safe. Speak to your home and garden expert for recommendations on how to fortify your home and lawn against ticks.
- Wear Protective Clothing: Clothing is your first line of defense when working or playing outdoors, especially in wooded or densely vegetated areas. Clothing can be treated with 0.5% permethrin, which will continue to protect even after several washes.
- Check Clothing: When returning inside, check clothing for ticks and promptly wash in hot water to avoid these pesky critters from migrating and attaching themselves later.
- Spray Insect Repellent: Using Environmental Protection Agency (EPA)- registered insect repellents can ward off ticks. However, be aware that some may contain OLE or PMD that should not be used on children under three years old.
- Protect Your Pets: Ticks enjoy hitching a ride indoors via pets and later transferring to you or your children. Check your pets carefully, paying close attention to hard-to-see areas whenever they return inside. You can also treat your dogs with tick prevention methods. See your veterinarian for suggestions for protecting your furry friends.
Removing Ticks Promptly and Safely
Check yourself, children and pets for ticks by both looking and feeling, especially in places like hair, armpits, back and belly buttons. If one is found, use the following steps for safe removal.
- Use clean, fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
- Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouthparts to break off and remain in the skin. If this happens, remove the bits with tweezers. If you cannot remove them easily with tweezers, leave it alone and let the skin heal. In most cases, the body will naturally expel tiny bits that may have been left behind.
- After removing the tick, thoroughly clean the bite area and disinfect with rubbing alcohol. Then wash your hands with soap and water.
- Never crush a tick with your fingers, as this can puncture the skin and further spread bacteria.
- Dispose of a live tick by putting it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet. Consult with your family practice doctor to see if tick specimen should be saved for testing.
I Don’t Know If I’ve Been Bitten. Should I Be Seen Anyway?
Tick bites are usually painless and oftentimes patients with tick-borne diseases don’t recall ever being bitten. This is due to the tick’s ability to inject an anesthetic into the skin, allowing them to feed undetected by its host. Often the first sign is the appearance of a bullseye rash that may occur after the tick has naturally dropped off. The rash typically has a red, circular appearance that becomes clearer in the middle of the ring. The rash may appear anywhere between 3-30 days after the initial bite and increases in size up to 12 inches across. It’s typically not itchy; however, it may feel warm to the touch. Other symptoms that may be noticeable early on are fever, chills, fatigue, body aches, headache, neck stiffness, dizziness, swollen lymph nodes and heart palpitations.
If untreated, new signs and symptoms of Lyme disease may appear weeks, months or even years following, including severe joint pain often found in the knees, numbness or weakness in limbs, impaired muscle movement and temporary paralysis of one side of the face (Bell’s palsy).
If you think you’ve been bitten and have signs and symptoms of Lyme disease — particularly if you live in an area where Lyme disease is common — contact a Lyme disease specialist.
Your Best Choice For Treatment
Treatment for Lyme disease is more effective if begun early, and Dr. Robin Ridinger has 25 years of experience in diagnosing and treating Lyme disease. Her broad scope of personalized functional medicine includes optimizing health, wellness, sleep, and nutrition, decreasing chemical and toxin exposure, and supporting whole-body detoxification. While successful treatment of Lyme disease oftentimes involves the use of antibiotics, Dr. Ridinger will monitor your progress closely and may incorporate a range of therapies, such as special diets, supplements, bioidentical hormones, and herbal treatments.
She understands the challenges, frustrations and fear confronting the journey to health and wholeness. Her compassionate and listening ear is ready to help answer any questions and get you on your path to happy and healthy living.
Ready to discover healing? Request an appointment at Premier Health and Holistic Medicine today.